Revenue Cycle
What is Revenue Cycle Management (RCM)?
Revenue cycle management (RCM) is the financial process utilizing medical billing software that healthcare facilities use to track patient care episodes, from registration and appointment scheduling to the final balance payment to ensure proper identification, collection, and management of revenues from patient services.
What is Healthcare Revenue Cycle Management?
Financial stability is critical for healthcare organizations to stay in the business of helping patients. They must properly collect and manage revenue to ensure profitability and economic viability. Equally important is having complete visibility of their revenue cycle and revenue generation practices and processes, including billing, payment, and claims processing. That’s where revenue cycle management comes in.
RCM is the process of managing all revenue-generation functions in a healthcare organization. It requires understanding the revenue cycle, which begins when a patient seeks the organization’s medical services and ends when the organization has collected all payments from the patient and/or their insurer.
The Revenue Cycle in Healthcare
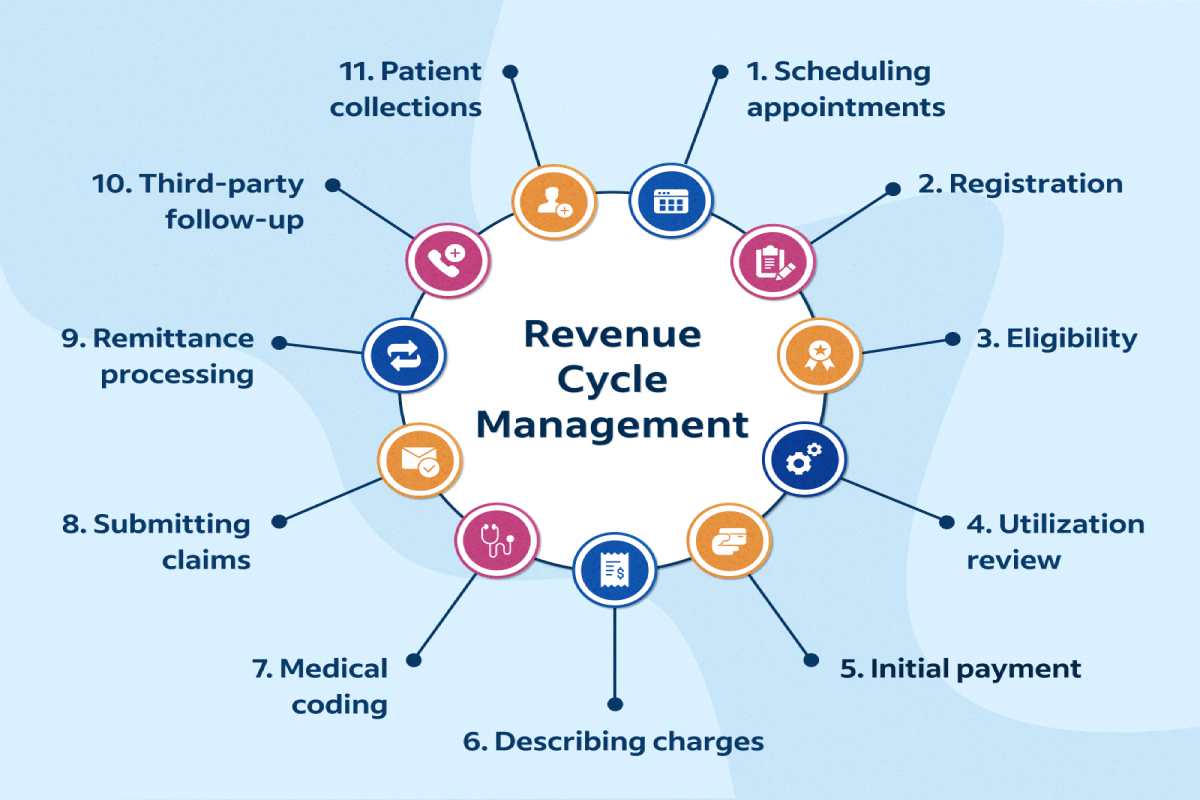
In healthcare, the revenue cycle includes all the administrative and clinical functions that contribute to capturing, managing, and collecting patient service revenue. The following activities are involved in the revenue cycle: charge capture, claim submission, coding, patient collections, preregistration, registration, remittance processing, third-party follow-up, and utilization review.
The Importance of Data in Revenue Cycle Management
RCM unifies the business and clinical sides of healthcare by coupling administrative data, such as a patient’s name, insurance provider, insurance coverage, and other personal information, with the treatment a patient receives, their medical history, and any available healthcare data (preexisting health conditions, allergies, lab test results, etc.).
Creating a patient account that includes data from the initial appointment setting can help simplify the organization’s {revenue cycle}. Preregistration — the collection of information before patient arrival — brings clarity into the cycle, reduces the probability of time-wasting rework, and helps optimize RCM.
Revenue Cycle Management and Insurer Communications
Communicating with health insurance companies is a critical component of RCM. When a patient schedules an appointment, the physician’s office or the hospital staff typically checks the patient’s reported insurance coverage before the visit.
After an insured patient receives treatment for a given condition and supplies any applicable copayment, a healthcare provider or coder categorizes the nature of the therapy using codes according to the International Classification of Diseases, 10th Revision (ICD-10). The hospital or care facility then sends the care summary with ICD-10 and Current Procedural Technology codes to the patient’s insurance company to see what portion of the care will be covered by insurance, with the patient billed for the remainder.
Benefits of Revenue Cycle Management (RCM) and RCM Systems
Proper RCM enables hospitals and other healthcare organizations to manage all functions associated with revenue generation efficiently. These functions might be administrative or clinical, and managing them makes identifying and collecting revenues from the patient services delivered easier.
An RCM system is essential for storing and managing patients’ billing records for efficient and error-free {revenue cycle} management. Many vendors develop RCM systems as standalone products or integrated with electronic health record (EHR) systems, including GE Healthcare, Accenture, Experian Health, Cerner, and Optum360.
An effective RCM system can reduce the time that lapses between providing a service to a patient and receiving their payment by interacting with other health IT systems — such as EHR and medical billing systems — as patients move through the care process.
Revenue Cycle Management And Value-Based Care
RCM systems facilitate the healthcare industry’s transition from fee-for-service to value-based reimbursement. The systems provide analytics enabling organizations to assess their patient population, see what portion suffers from chronic diseases, monitor claims data, and pinpoint abnormalities. They can also report healthcare costs and patient satisfaction to insurers, increasing the chances of receiving full reimbursement from payers and minimizing the chances of claim denials.
Integrating RCM and clinical workflows through a customized EHR implementation can help a healthcare practice streamline efficiencies. See how a customized EHR implementation with RCM boosted a practice’s growth.